Well, I am not really sure when it all started but I am sure when we figured out what was going on. It was July 22, 1984. Forty years ago today. In some ways you could say it was a good day, because I did not die. In other ways, it was a bad day, because I nearly died and also found out what had been going so wrong with my body for some time.
Though as I said I am not sure when it all started, I do know that for a few months my health was deteriorating. I had told my father, who was a doctor (though he did research at the NIH and was not a practicing clinician), that I just did not feel right. I had been mentioning this for a month or more. But in July I mentioned it more. And he did not seem to think there was anything to worry about.
I was a pretty active kid then and was quite athletic – at least – before my body started having issues. I think this is partly why my dad thought that I must be fine. I played soccer, baseball, street hockey and various other sports.
I had even made the Varsity Baseball team as a sophomore and had done OK.
As an aside, it is kind of fun to see discussion of how I played baseball with Anthony Dilweg who went on to play QB for the Green Bay Packers. Anyway … back to the story. And as another aside, it is cool to me that I am still in touch, at least a tiny bit, with a few people from this team (e.g., Tom Nylen, Andy Keith).
Anyway – more on that in a bit. It was now the summer. And I was still pretty active. Most days went something like this. I was taking Driver’s Ed classes in downtown Bethesda getting ready to get my drivers license. I would bike to the class. Then I biked over to work at the Carey Winston Company where I did data entry, in a job that my friend Ross Kaminsky helped me get. Then I would bike to my High School (Walt Whitman) where I had baseball practice for a summer league team. And then I would bike home. On days when I had a game I think I would bike home, get my uniform on, and then either bike (if the game was nearby) or get a ride from my mom or brother. With all this activity it made a little bit of sense that I might also feel tired all the time, and also that I was pretty skinny. So I think my dad thought “Oh, he must be fine.”
But I knew something was up. Something definitely was not right. And a few days before July 22, I had decided I was going to force the issue. In part, this was because I was feeling worse and worse. But also in part it was because my brother and I had our first backpacking trip planned, with a friend Matt Smith. I was excited about this but also a bit worried due to my health issues. Basically, I was just really really tired. That was the number one symptom. Just crazy tired. And I felt weak. Really weak. (I had other symptoms but more on those later). So here I was – getting ready for my first real outdoor adventure – to hike up Old Rag Mountain with Matt (and Eagle Scout) and my brother and to camp overnight and then get picked up the next day. This did not seem like an ideal time to do that, given that I felt like I could barely walk some of the time.
You see, despite being really active, and doing OK at some of these activities, I just knew something was wrong. In retrospect, something had been going wrong for actually quite some time. Amazingly, I even found that I discussed this pretty openly with people writing stories for our school paper about the Varsity Baseball team in the Spring. For example:
I had a good throwing arm as a pitcher so I could do ok. But I was tired all the time. Like really really tired. For every game. And things had been getting worse over the Summer. So – even though my dad did not think something was wrong, I did. So as I said, I was going to force the issue.
But then somewhere July 18th or 19th, I was the starting pitcher for our team in a baseball game and I pitched phenomenally well – a two hit shutout. I felt awful through the whole thing, but the result was excellent. And I felt like, if I could do that, I must be fine. So we decided to go ahead with the backpacking trip.
So – anyway – back to the summer league game. I pitched well and decided that it was OK to go on this trip. Here is what I wrote about that in a school essay (with corrections from my English Teacher)
This was unquestionably one of the dumbest decisions I have ever made. My mom and dad drove us to the trailhead for Old Rag Mountain, I think on Saturday morning. And then eventually me, Mike and Matt headed up the mountain.
And here is where the shit truly hit the fan. I did not tell you one of the key other symptoms I had, which was thirst. Just devastating thirst. I could not imbibe enough liquid. I basically drank my 2 day supply of water in like 30 minutes and then basically polished off as much of the water of my companions that they would let me have. So just like that, we were out of water basically. Oh, and I was also peeing all the time too. Yay.
Here is what I wrote about that in that school essay mentioned above (with corrections from my English Teacher)
Somehow, yes, we made it up Old Rag Mountain and ended up sleeping near the top. The whole time, I felt like I was dying. And in fact, I was. Somehow I made it through the night. Also – despite what I said in the essay – my brain was not functioning particularly well and I really do not remember much about that night. Maybe my brother or Matt Smith can chime in at some point. I vaguely remember that we could not find any water and that Matt had brought some adult beverage to drink which he consumed and my brother had to try and figure out how to deal with the drinker and the dying person at the same time. Anyway – it was not a good night. But I did make it through the night.
I do not have any pictures from the trip but if you are interested – here is some information about hiking up Old Rag:
From https://www.nps.gov/thingstodo/old-rag-summit-berry-hollow.htm
Although I was alive the next morning, I was not doing well. I was so so so so so so so tired. And so confused. And so so so so so so thirsty. And since we were basically out of water, things were not good. On our hike down the other side of the mountain, I started drinking from puddles and trickling baby streams of water. Anything I could find. I slurped from muddy puddles like a dog. And I could barely move. My body hurt like never before. My legs were so weak. And my brain was not all there.
Finally we got down to near where we were to be picked up and there was a house and maybe a farm down there. But most importantly, something there I think saved my life. A hose. I turned it on. And drank. And drank. And drank. And drank. And then peed. And drank some more. And then peed more. And then drank. We waited there for a bit for Matt’s parents to pick us up but the water I got from that hose I am fairly certain saved me.
Clearly, the next thing to do was to go to the hospital. But that was not to be. We got dropped off in the early evening and my dad’s lab had some sort of party that we went to. I barely remember this but I do know they were playing volleyball and despite this being one of my favorite activities normally I did not play. I just sat on the ground nearby, not moving. And at some point I think my parents / my dad realized there was in fact something really wrong.
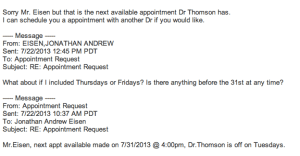
I vaguely remember that we left the party and went to a drug store (I think People’s) to buy a urine sugar testing kit. And at some point we tested my urine and it was off the scale – literally filled with sugar. And so my dad said something to the effect of – “You have diabetes, we have to go to the hospital.” And off we went to Bethesda Naval Hospital to the emergency room (because my dad worked at the NIH and was a commissioned officer in the Navy, we got our medical care there).
I think I was pretty much not fully alert during all of this. But eventually I was transferred to a bed in the pediatrics unit and then spent many days in the hospital recovering and learning how to treat myself as a diabetic.
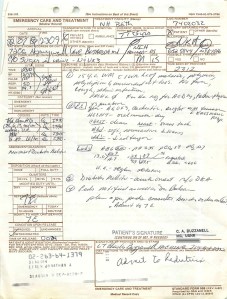
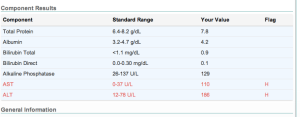
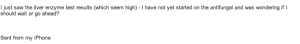
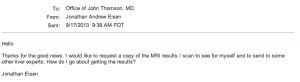
In many ways, I was lucky to be alive. I easily could have died on that backpacking trip and if I had not found that hose at the end of the trip, I think I might have died out there. I was in rough shape and things had been going poorly for a while. I looked like a famine victim. I had lost something like 40-50 pounds over a few months. I was in full blown diabetic ketoacidosis and slipping away until they gave me IV fluids and eventually insulin in the ER. Here is the page from my admissions (missing some details on various tests they ran, but suffice it to say I was not doing well)
So in retrospect again, it is pretty crazy that I had not gone in to get checked out before this crisis. Certainly, my dad, an endocrinologist (though again, one who did research in a lab at the NIH and did not practice) probabiy should have caught this earlier. We even had just been in Quebec where my dad was attending the Endocrine Society Annual Meeting and I had been surrounded at various events by world leading endocrinologists.
At dinners, I was getting up all the time to pee, but I did not announce this. And if anyone noticed me seeming fidgety, they probably either thought I was a typical bored teenager or maybe thought I was on drugs.
See https://academic.oup.com/edrv/article-abstract/5/2/370/2548924?redirectedFrom=fulltext
I note – one of the issues with my deteriorating health was that it came along slowly, over many many months. It was like the proverbial frog in the frying pan story – I just kept adjusting and adjusting and adjusting my baseline expectations about what was normal and what was OK slowly over time. And I did not even notice really all the issues. The one I noticed most was fatigue and weakness. What I did not really notice, which seems really bizarre in retrospect, was two key other symptoms that had gotten worse and worse and worse over the months. These were thirst, and the need to pee all the time.
For example, by that time in Mid July, my daily routine was not quite as I laid it out above. This was the daily routine with the full details with the extra new details highlighted with underlining and bolding.
Most days went something like this. I got up in the morning early because I had to pee. Then I went downstairs and made a large two liter pitcher of orange juice from a frozen can. And I drank most of it. I was taking Driver’s Ed classes in downtown Bethesda getting ready to get my drivers license. I would bike to the class. Although it was only about a 20 minute bike ride to the class, I would stop on the way at Montgomery Donuts to get a drink and use the bathroom.
Then I would go to class where every 20 minutes or so I would get up to pee. Then I biked over to work at the Carey Winston Company where I did data entry, in a job that my friend Ross Kaminsky helped me get. While working I would spend a lot of time getting up to use the restroom and to buy sodas to quench my thirst. Then I would bike to my High School (Walt Whitman) where I had baseball practice for a summer league team. And during practice, or even during games, I would have to sneak off all the time to pee in the bushes and to also get a drink. And then I would bike home.
Oh and of course, since I did not know I was a diabetic, I was probably making things worse by drinking sweetened drinks all the time. Yes, they seemed to quench my thirst. But they just added more sugar to the fire.
And again, in retrospect, I had been “building” up to this for some time. During the second semester in high school that Spring, I remember having to pee between classes a lot. I remember even being stressed during classes about needing to pee and get excused all the time even before class.
Yes, clearly, it would have been better to have figured things out sooner. But somehow, I did not die. And that was a good thing. As I was in the Navy Hospital, trying to comprehend what this all meant, for reasons that I am not entirely sure of, I did not spend a lot of time lamenting about “Why me?” I mean, sure, it sucked. And sure, I knew my life was altered. But I somehow just wanted to move forward, get on with my life, and deal with the altered reality.
This moving forward thing in part I think came from my general nature. But there were also a few things that happened while I was in the hospital and shortly after that really really helped my perspective and I mention some of these in the next few paragraphs.
One thing that helped me immensely once I was in the hospital was that the pediatrician who took care of me was Dr. Marion Balsam, who happened to be the mom of a friend Ross Kaminsky. I had hung out a lot with Ross a few years before that and knew his mom and this was just remarkably comforting. Plus she was a just phenomenal doctor.
Another thing that really really helped me move forward was the fact that there was a kid in the bed next to me who had brain damage from some type of accident. I realized that things could be much worse than having to take shots and deal with a defective pancreas.
But even with those two things helping me in ways, I was still not fully in a good place mentally. For example, I was at the Bethesda Naval Hospital and alas I had a painful conversation with one of the orderlies who was taking care of me on Day 2 or so. You see, I had dreams of going to the US Naval Academy and playing baseball there and we were discussing this. I had even had a discussion with the Navy Baseball Coach and had either taken or at least signed up for the ASVAB test (I can’t remember anymore). Alas, the orderly then, matter of factly, told me, you can’t join the Navy as a diabetic. Well, shit, there went that dream.
So, you know, even though physically I was starting to feel better than I had in months (IV fluids and insulin for the win …), mentally I was still not in a completely great place. But fortunately I had a lot of visitors (my family and friends must have worked hard to keep me occupied). This was really really uplifting. Someone – possibly Ross – even took me on my first “outing” to get out of the hospital ward. We went bowling at the Navy Bowling alley nearby).
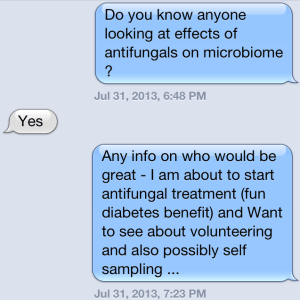
And one of those visitors definitely changed my mental state. You see there was a girl who I had a bit of a crush on who came to visit me in the hospital because it turned out she was also a diabetic (I had not known that). And, well, eventually we developed a relationship – my first real girlfriend. Honestly, I think she probably is more responsible for me being alive today than anyone else because she taught me about diabetes and I wanted to get my diabetes in control to show her that I could do it.
A fourth thing that definitely helped me was that my family had a trip to Alaska planned for a few weeks from when I went in to the hospital and Dr. Balsam encouraged us to still go on the trip. Since my dad was a doctor, in theory he could help take care of any issues that arose. So I had incentive to show that I could manage my diabetes as soon as possible so they would let me go on this trip. And we did. And the trip was incredible. Here are a few pics from that trip:
Although another time I will tell the story about how I cracked a rib and my dad was worried I had punctured my spleen when I crashed into a fire pit while playing frisbee at a campsite in the middle of nowhere. And we cut our trip short by a day to get me to a hospital for a check up. But another time.
A final thing that helped me move forward is, well, that the medicine (insulin basically) was like magic. When they first gave me some in the hospital, I literally think I could feel my body starting to wake up and work again. And since I was almost 16 and had been a science dork of sorts, I actually already knew what insulin was and what diabetes was. I had not imagined I would get it of course, but knowing what it was all about certainly helped too.
Anyway, 40 years ago today, I got knocked down. But I got back up. And it has certainly not been easy. But I am still here. Always looking forward. And looking backwards, from a historical point of view, but rarely from a “why me” point of view. I truly feel blessed to have had these extra forty years. Here’s to forty more.
UPDATE 7/25/2024
Got some nice responses to my post at various social media sites and thought I would share links here.